The Pandemic’s Health Impact on Southeast Asia
By Dominique Fraser
Published on 17th November 2022
Read in 6 minutes
After two-and-a-half gruelling years, Southeast Asia has opened its economies and borders and is learning to live with COVID-19. The Asia Society Policy Institute and Asia Society Australia are therefore bringing our long-running Southeast Asia and COVID-19 project to a close. As we do so, we briefly revisit earlier project analysis of the pandemic’s effect on the region’s geo-politics, economics, and society.
The COVID-19 pandemic had a horrific human impact on Southeast Asia as it did in much of the world. According to official numbers, by the end of 2021, a little over 300,000 Southeast Asians had lost their lives to COVID-19. As these numbers are likely severely under-reported, looking at excess deaths reveals a more accurate – and much more dire – picture. Data from the World Health Organization (WHO) suggests more than 1.2 million people had died due to the pandemic by end 2021, four times as many as the official numbers indicate (see Table 1).
Even this raw data, of course, can never fully capture the suffering caused by the pandemic. Among those who died were courageous front line health workers. Households lost breadwinners; children were orphaned. The poor often died outside over-loaded hospital systems. The terrible Delta wave that ravaged Jakarta left few families in the city untouched by loss and sorrow.
Table 1
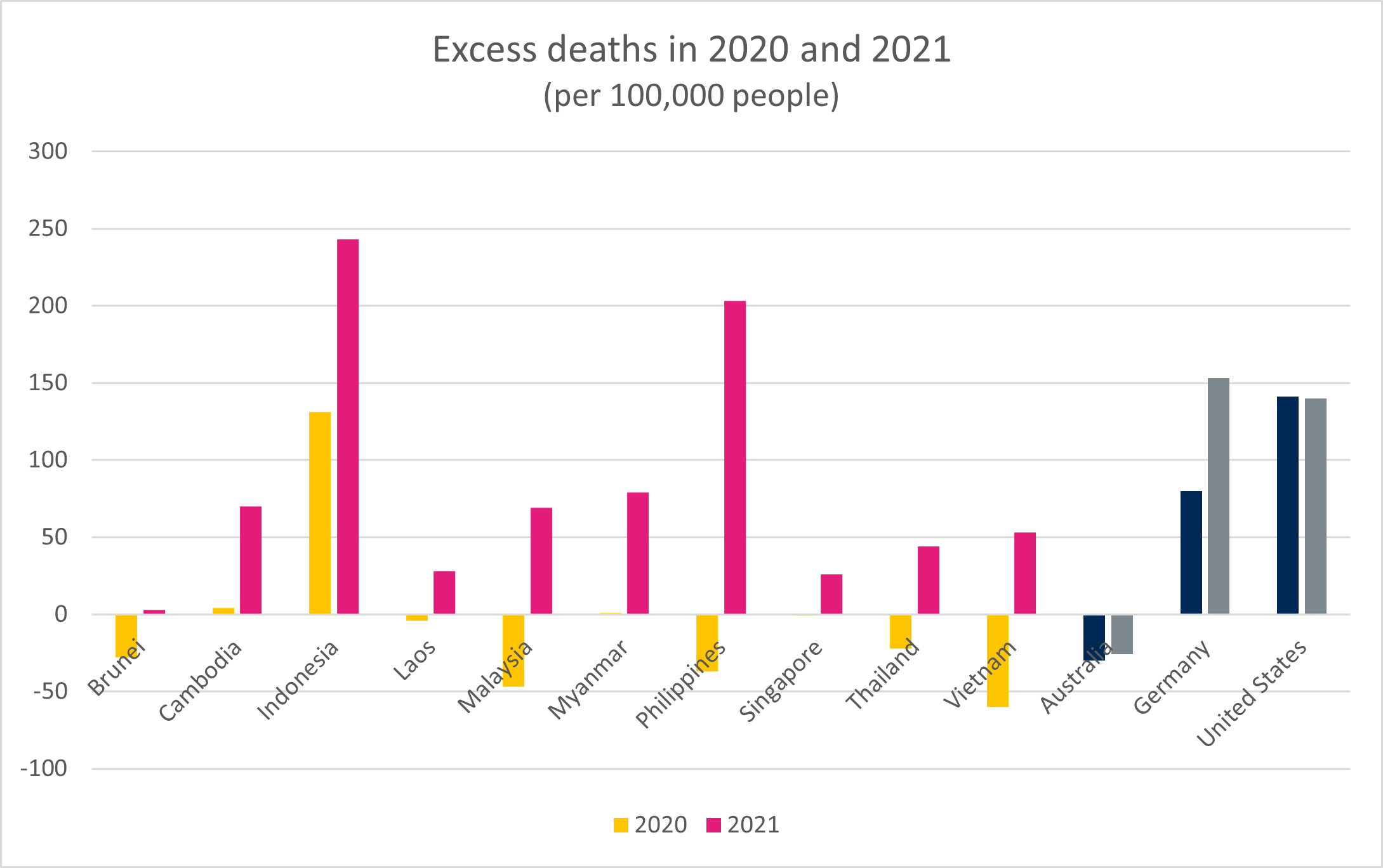
Source: WHO
Looking at excess deaths reveals that while much of the region managed the first wave starting in March 2020 (see Table 2) reasonably well, especially compared to the United States and much of Europe, it struggled to contain the virus in 2021.
As the virus spread to the region from January 2020, with Thailand the first to record a case outside of China, most leaders acted quickly to introduce effective social distancing measures. A study in Nature, aimed at evaluating the effectiveness of different measures to contain the pandemic, shows what many in the region did well in that first year: quickly shutting international borders and banning domestic travel, closing schools and entertainment venues, communicating effectively with their populations, and providing financial assistance to those in need (carried out mainly through cash payments and tax breaks). A different study highlights that moving quickly, as the region did, played a vital part in its success. Some have further argued that Southeast Asians were more compliant than people elsewhere in the world due to cultural factors.
Indonesia was a notable exception. President Joko Widodo announced the country’s first two COVID cases on 2 March, by which date experts assumed that a “silent epidemic” was already well under way, having gone unnoticed due to a lack of testing and tracing. Jakarta was slower than elsewhere in the region to impose a lockdown and President Widodo resisted closing borders. President Widodo argued Indonesia, especially its poorest citizens working in the informal economy, could not afford to lock down harder. Still, the decision to prioritise the economy led to large excess death numbers in 2020, almost on par with the United States.
Table 2
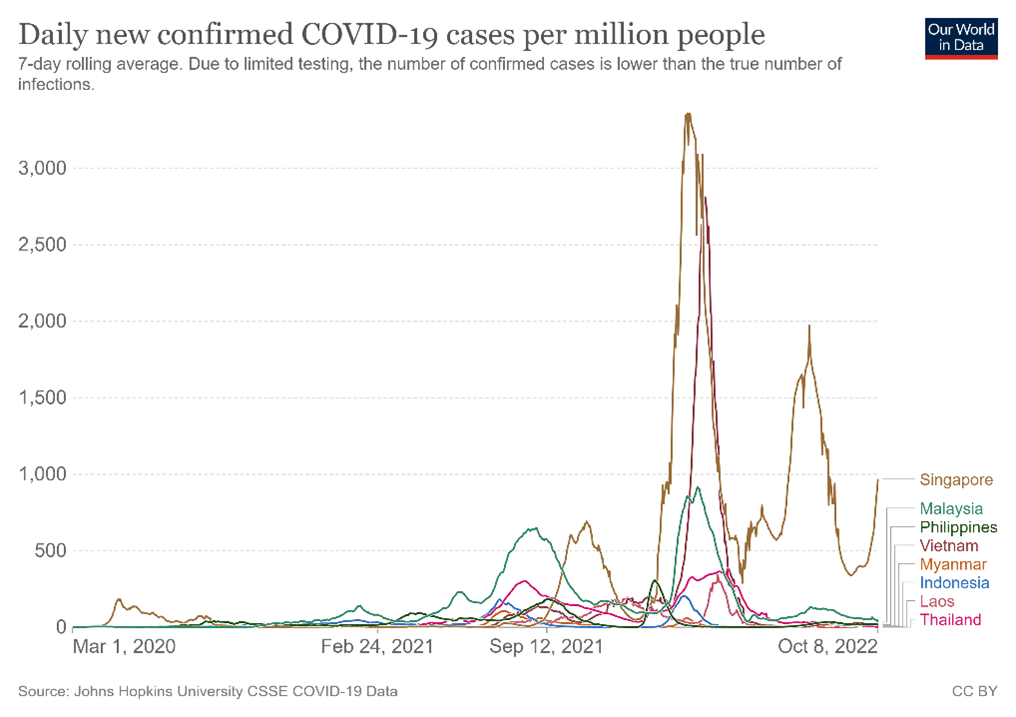
Source: Our World In Data
As the second, Delta-fuelled wave swept across the region from mid-2021 (see Table 2) and governments loosened restrictions in a bid to boost economic activity, the region struggled to contain the virus. This was particularly pronounced in Indonesia, which briefly emerged as the world’s COVID epicentre in mid-2021 and where more people died from the pandemic than elsewhere in the region relative to their population (see Table 1). As Richard Maude wrote at the time for this project, President Widodo had pinned “his hopes on a nation-wide vaccination program and hasn’t wanted to damage Indonesia’s fragile recovery from last year’s recession”.
The emergence of Omicron in early 2022 led to a third wave and an explosive case load (see Table 2), but thankfully no proportionate increase in loss of life thanks in part to lower mortality rate and by then high vaccination rates.
Vaccinations
High vaccination rates were only slowly achieved, however. As Maude wrote in June 2021, the slow and patchy vaccine rollout led to further suffering in the region. In many parts of Southeast Asia, the vaccine rollout began in early 2021 thanks to sales contracts with and donations by China. However, some factors prevented a quick and smooth vaccination campaign. These included overall low stock and a globally unequal distribution of vaccines, struggling healthcare systems, challenging geography, distrust of Chinese vaccines, and in some cases distrust of government. This last point has been particularly salient in Myanmar, where the military had deposed the democratically elected government in a coup on 1 February 2021.
Table 3
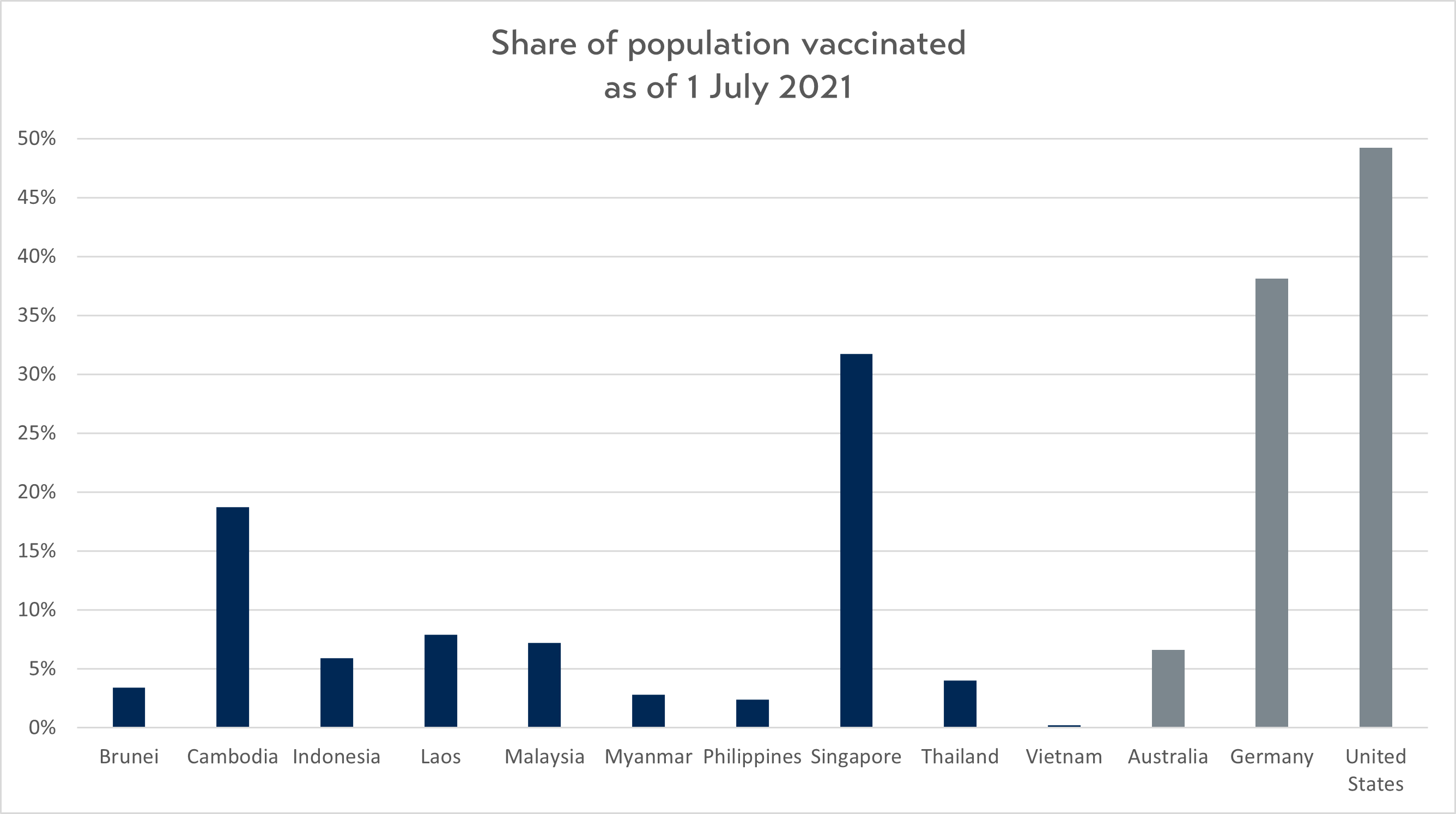
Source: Our World In Data
While by 1 July 2021, nearly half the population in the United States was fully vaccinated and nearly 40 percent in Germany, in Southeast Asia, the rate was just over 5 percent (excluding Singapore, where nearly one third of Singaporeans had been vaccinated) (see Table 3). While Indonesia has relied heavily on Chinese vaccines, in particular Sinovac, the rest of the region has used a combination of different vaccines. Chinese vaccines have been less popular for booster shots, due to their lower effectiveness.
A perhaps surprising early vaccination success story was Cambodia, where nearly 20 percent of the population had been vaccinated by mid-2021 and which today boasts the region’s third highest vaccination rates. Cambodia quickly bought large quantities of Chinese vaccines and received sizeable donations from China. It then implemented a fast and effective vaccination campaign, which focused on location rather than age groups and included vaccine mandates for large sections of society.
On the other end of the spectrum was Vietnam, where slow vaccine procurement, relative neglect by China, a distracting leadership change, and perhaps a belief that the hitherto successful measures would keep future waves at bay, meant that less than 1 percent of the population was vaccinated by mid-2021.
Thanks to a “revolution in vaccine production and donation” starting in mid-2021, the overall picture is much rosier today with an average of two thirds of the population across the region vaccinated with the initial two doses (see Table 4). This was made possible by commercial sales and donations to the region flowing through the COVAX mechanism, to which the United States, China, and the European Union have been the largest donors, as well as bilateral donations coming from the United States, which has overtaken China as the largest bilateral vaccine donor to the region.
The Quad Vaccine Partnership, which had promised to deliver 1 billion doses to the Indo-Pacific by the end of 2022, has been a disappointment, with its first delivery made to Cambodia as late as April 2022, at which point there was already an “oversupply” of vaccines in Southeast Asia.
Table 4
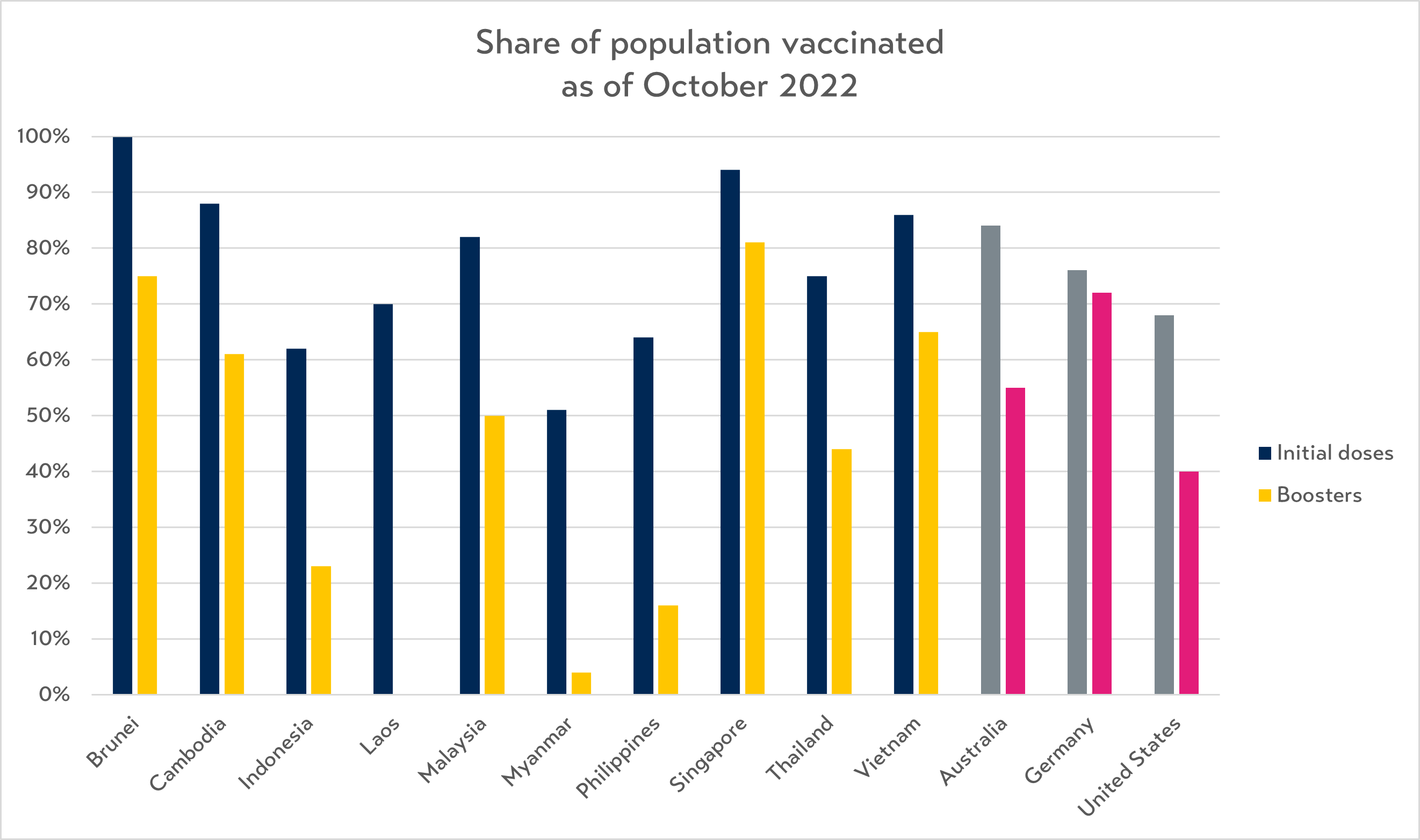
Source: Our World In Data
Thailand was the only country in the region which produced substantial quantities of vaccines (AstraZeneca), while Indonesia and Malaysia had “fill and finish” deals with Sinovac. A number of local companies and universities are currently working on their own vaccines, including in Thailand, Indonesia, and Vietnam, with clinical trials in Stages II and III.
With overall high vaccination rates, some countries lag when it comes to booster shots, in particular Myanmar, the Philippines, and Indonesia. In Myanmar, the health care system has all but collapsed amid neglect by the military regime, civil conflict and the arrest of healthcare workers. In the Philippines, general hesitancy for vaccines has in the past hampered vaccine drives and the high uptake of the original COVID vaccine doses was a notable outlier. In Indonesia, a lack of supply, an uneven vaccine rollout, and confusion over whether booster shots were free may have contributed to the low percentage of the population opting for a booster shot.
Preparedness
As the world is slowly entering a post-COVID era, countries must invest to be prepared for any potential future epidemics. According to the Global Health Security Index, which assesses countries’ health security and capabilities, Southeast Asia is in decent shape (see Table 5). Giving 195 countries a score out of 100, the global average is just 38.9, with only Cambodia (31.1) and Laos (34.8) scoring below the average. According to the Index, Thailand (68.2) is the region’s best prepared country, beating high-income Germany (65.5).
Table 5
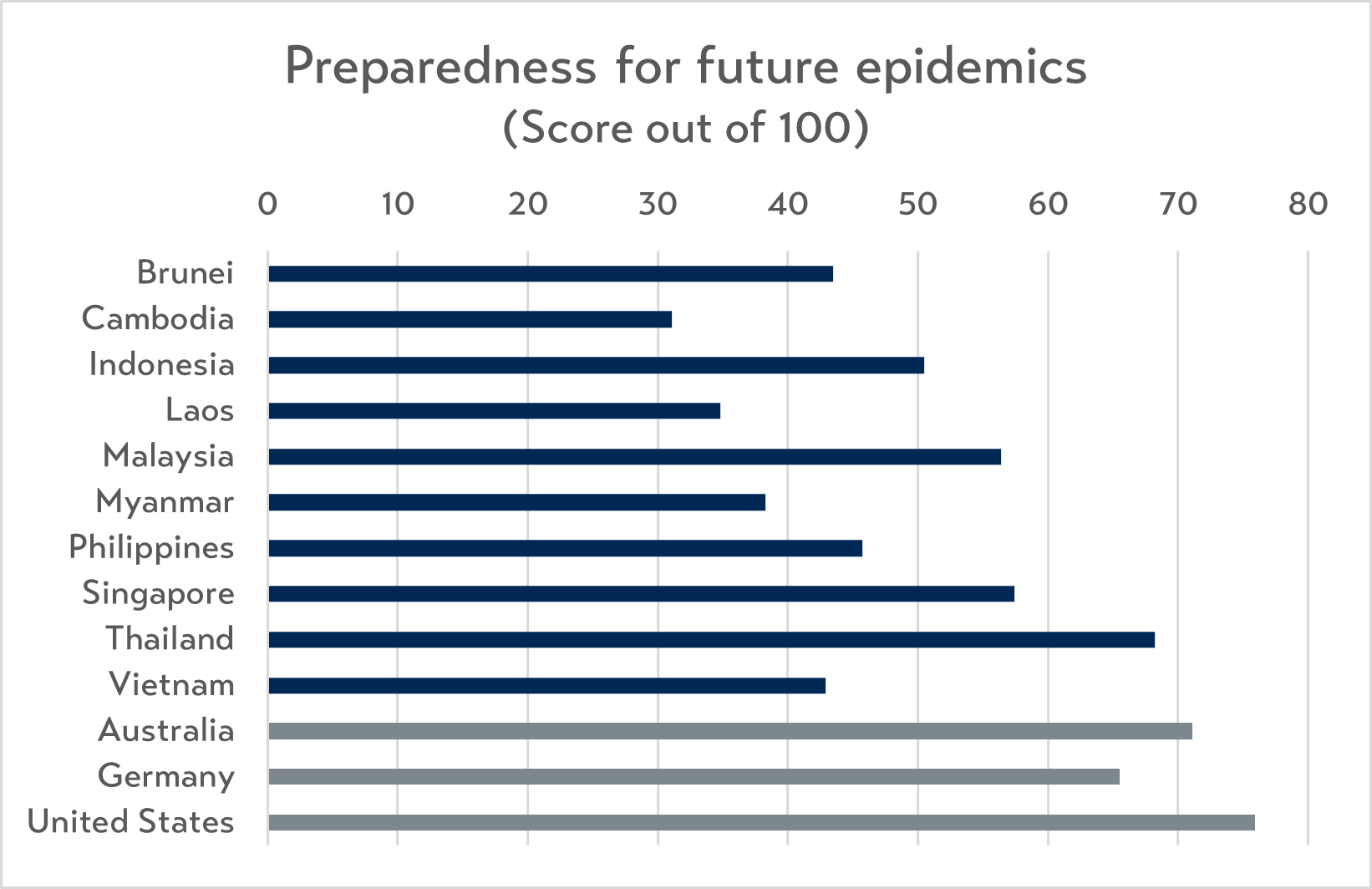
Source: Global Health Security Index 2021
Nonetheless, members of the Malaysian Health Coalition wrote for this project in March 2022 that “no Southeast Asian country has begun concrete measures to reform or strengthen their national health systems (beyond reports, white papers, or political promises).” To improve preparedness for future health shocks, the authors recommended that countries in the region: a) increase and diversify health financing to make it more sustainable and equitable; b) invest in the healthcare workforce through training and offering career progression; and c) build digital health infrastructure.